Gd Induced Disease
Gadolinium Storage Condition
any individual who receives an MRI with gadolinium contrast
Gadolinium, a heavy metal used in gadolinium-based contrast agents (GBCAs) for MRI scans, while initially thought to be fully excreted through the kidneys, actually retains in the bones, brain, skin, and organs of those who receive it. Detecting gadolinium in the body often requires gadolinium-specific tests. Deposition in organs can be detected during autopsy, but in living patients, proving deposition can be challenging without invasive tissue samples. This is because urine excretion often drops to zero in patients with a limited number of gadolinium-based MRIs. However, provocation tests and chelation can reveal retained gadolinium levels.
If you received a GBCA and do not exhibit symptoms or an obvious disease state, according to Dr. Richard Semelka, you have Gadolinium Storage Condition. This term describes individuals whose body holds onto the metal without experiencing pain, cognitive issues, or other signs of toxicity. However, this does not mean the body is wholly unaffected—gadolinium is still a foreign toxic substance, and its long-term impact is not fully understood.
To read more about the individuals who do experience symptoms, see Gadolinium Deposition Disease (GDD).
Gadolinium Deposition Disease
aka: Gadolinium Toxicity or “Symptoms Associated with Gadolinium Toxicity”
Patients with normal renal function injected with gadolinium based contrast agents are the first people in human history to endure gadolinium deposition disease (GDD).
Onset: immediate or within the days-weeks-months following injection; onset can be the first injection or subsequent injections
Symptoms: due to Gd’s systemic distribution, there is an array of symptoms including but not limited to neurological, muscle weakness, fasciculations, pain, and burning in the skin, organs or tissues that did not exist prior to the GBCA injection
The medical industry recently came out with its own classification of gadolinium toxicity called, “SAGE,” or Symptoms Associated with Gadolinium Exposure (McDonald et al, 2021). To those who have suffered with this disease for decades, this is a misnomer for the following reasons:
-
Gadolinium causes a chronic, difficult-to-reverse illness characterized by a single, continuous toxicity rather than isolated symptoms. Viewing gadolinium toxicity as a collection of unrelated symptoms risks misdiagnosis and ineffective treatments, whereas chelation with immune modulation offers the highest success rate for GDD (Semelka et al., 2022; Patient Reports).
-
“Associated” implies loose correlation, as opposed to direct causation. Gadolinium causes toxicity. In the case of lead or mercury poisoning, we accurately refer to the condition as "lead poisoning" or "mercury poisoning," recognizing their toxic effects on the body, down to the cellular level. The same clarity should apply to gadolinium toxicity, as it too involves direct toxic effects.
-
Patients are never simply exposed to gadolinium; rather, it is directly injected into their bloodstream. This introduction of a lanthanide heavy metal causes immense strain on the body, which is equipped only to process essential minerals. In response, the body attempts to expel gadolinium through all available means, including nails, hair, breast milk, urine, feces, and more. Some patients report vomiting or excessive sweating immediately after receiving gadolinium — natural defense mechanisms to eliminate toxins.
Dr. Semelka aptly coined the term "Gadolinium Deposition Disease," highlighting how gadolinium deposits in the body and triggers a previously nonexistent disease. As patients who first raised public awareness, we recognize "Gadolinium Deposition Disease" and "Gadolinium Toxicity" as the most accurate and honest terms.
Read about the most common GDD symptoms on Dr. Richard Semelka’s blog.
For decades, patients have suffered immensely due to GBCAs, and the name of their condition should honor their lived experiences.
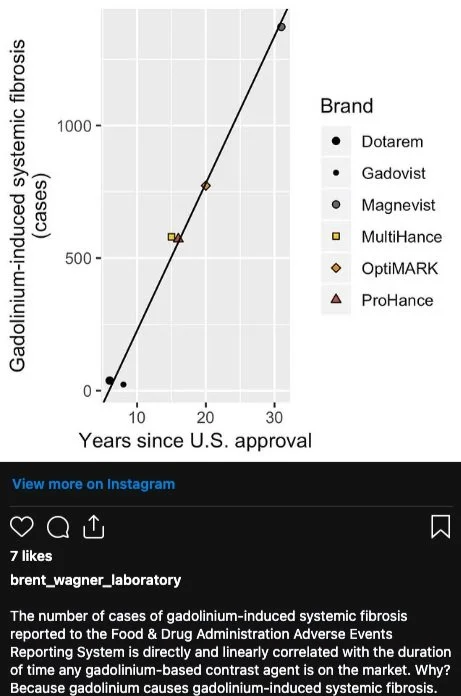
Nephrogenic Systemic Fibrosis
aka: Gadolinium Induced Systemic Fibrosis or Fibrosis
“The ultimate therapy is one that stops fibrosis before it ever begins” - Shawn Cowper
Onset: immediately to years later
Symptoms: irreversible and unstoppable hardening of the tissues, skin, and organs, which proves fatal
The Problem: The medical community claims that no cases of NSF (Nephrogenic Systemic Fibrosis) have been reported in the past decade. However, this is inaccurate. Multiple patients with normal kidney function have developed systemic fibrosis after limited exposure (1–8 scans) to newer macrocyclic gadolinium-based contrast agents (GBCAs). These cases are no longer publicly reported, despite patient efforts to get recognition.
The narrative that NSF is solely linked to kidney function shifts blame onto patients, ignoring the root cause: gadolinium poisoning. Systemic fibrosis only occurs due to gadolinium exposure. Millions of kidney failure patients never develop NSF simply because they are not injected with gadolinium. If NSF were a disease of the kidney, we would observe it in a much broader population of kidney disease patients. Every case of systemic fibrosis is caused by gadolinium-based contrast agents—not kidney function.
Anaphylaxis / Immediate Death
aka: Hypersensitivity Reaction, Allergic Reaction
Onset: immediately
Symptoms & The Problem: Hypersensitivity reactions to gadolinium contrast dye range from mild symptoms like itching or hives to life-threatening anaphylaxis that can lead to cardiac arrest or death. For some patients, exposure to gadolinium can have immediate and devastating consequences, making it critical for healthcare providers to prioritize safety measures and patient screening.
One recent, high-profile example is the story of Michel Blanc, a renowned French actor, writer, and director, who died immediately upon gadolinium-based contrast agent injection during an MRI. His death serves as a stark reminder of the dangers posed by these substances. When asked about the known risks, many radiologists insist they cannot test patients for gadolinium allergies, citing concerns over "too many false positives" (Richard, 2024). This statement speaks for itself. The reason for these false positives is clear: no human body inherently "likes" a foreign toxic substance like gadolinium, as it is not naturally compatible with human biology.
Considering even a single exposure can result in fatal outcomes, failing to test pre-emptively for gadolinium reactions does not even offer patients the chance for prevention.
Excerpts from Michel Blanc’s Public Death Announcement
Multiple Myeloma / MGUS
aka: bone cancer
Multiple myeloma (MM) is a type of cancer that forms in plasma cells, a crucial part of the immune system that helps fight infections by making antibodies. The disease disrupts normal bone marrow function, leading to problems with blood cell production, weakened bones, and impaired immunity. Plasma cells in multiple myeloma become abnormal and grow uncontrollably, producing proteins that can harm the kidneys and other organs (Korde, et al., 2011).
The Problem: Emerging evidence suggests a potential link between gadolinium-based contrast agents (GBCAs) used in MRI scans and the development or progression of multiple myeloma. Studies, including a study published in Blood, have shown that GBCAs can promote the growth of myeloma cells in both laboratory and animal models (Fulciniti et al., 2009). This is concerning for gadolinium toxicity patients, some of whom have undergone bone marrow biopsies revealing markers of monoclonal gammopathy of undetermined significance (MGUS), a precursor condition to multiple myeloma (Korde et al., 2011).
The bone marrow is responsible for producing blood cells (red cells, white cells, and platelets) and stem cells, which are essential for tissue repair and immunity (Fulciniti et al., 2009). When heavy metals [like gadolinium] accumulate in the bone, they may disrupt these processes, potentially contributing to conditions like MGUS or even multiple myeloma (Durie, 2015).
Mast Cell Activation Syndrome
aka: MCAS
Mast Cell Activation Syndrome (MCAS) is a condition where the body’s mast cells—immune cells that release chemicals like histamine during allergic and inflammatory responses—become overactive and dysregulated, leading to widespread symptoms such as severe allergic reactions, inflammation, and chronic multi-system issues (WebMD, 2024). The link between MCAS and gadolinium, a heavy metal that accumulates in bone & other tissues following exposure to MRI contrast agents (Tweedle, 2022), is becoming more evident among patient reports. Since mast cells originate in the bone marrow, gadolinium’s persistent presence in bone may interfere with immune cell development or regulation. Like other heavy metals—such as mercury, lead, cadmium, and bismuth—gadolinium can disrupt normal cellular processes, potentially triggering mast cell activation and leading to excessive histamine release and chronic inflammation (Bent et al., 1992; Kempuraj et al., 2010). Over time, these disruptions can contribute to inflammatory conditions and even autoimmune disorders (Suzuki et al., 2011).
Patients exposed to gadolinium-based contrast agents (GBCAs) frequently report the onset of MCAS symptoms, such as heart palpitations, flushing, and gastrointestinal distress, shortly after exposure. While these symptoms may initially seem short-term, gadolinium’s persistence in the body often extends the inflammatory response. As Dr. John Gannage explains, “If the body is continuously exposed to toxins or other substances that it perceives as threats, the mast cells create a chronic inflammatory response through the release of several different mediators” (Gannage, 2024). This prolonged exposure and systemic inflammation can make it difficult for patients to achieve symptom relief, due to a cycle of reliance on mast cell stabilizers and anti-inflammatories until more gadolinium is removed through chelation.
In the video above, at timestamp 34:12, Dr. Anne Maitland, MD, PhD, highlights that individuals with Mast Cell Activation Syndrome (MCAS) are more likely to react to contrast dyes. She explains that facilities often pre-treat patients with medications to prevent immediate allergic reactions. However, this approach overlooks a critical issue: gadolinium, a rare earth heavy metal, can persist in the body long after the pre-treatment wears off. This raises the question: what happens when the drug suppressing the allergic response wears off, but gadolinium remains deposited in tissues, continuing to trigger mast cell activation? Further studies need to explore the link between Gadolinium Deposition Disease (GDD) and MCAS.
More article discussing the link between MCAS and gadolinium-based contrast agents:
Heavy Metal Toxicity and Mast Cells
Dr. Kelly McCann discusses how exposure to heavy metals like mercury, lead, cadmium, and bismuth may trigger inflammatory responses, mast cell activation, and histamine release.Mast Cells and Gadolinium Toxicity: Is There a Connection?
This article explores the potential link between gadolinium exposure from contrast agents and mast cell activation, suggesting that gadolinium may act as a trigger for mast cell degranulation.Heavy Metals, Mast Cell Activation, and Histamine Intolerance
This article from Histamined examines the connection between heavy metal exposure and mast cell activation, highlighting how metals like mercury and lead can contribute to histamine intolerance and inflammation.Mast Cell Activation Syndrome (MCAS) and Gadolinium Toxicity
Dr. Richard Semelka discusses the overlap between acute hypersensitivity reactions and gadolinium deposition disease, highlighting the role of mast cell activation.